Fertility Centre
Fertility Care Centre at Evercare Hospital Dhaka
Evercare Fertility Centre is one of the fewest and best fertility centre in Bangladesh. The centre has established itself as one of the most successful IVF programs in the country, offering international standard treatment in an environment of genuine care, warmth and support while maintaining total patient confidentiality. We assist couples with difficult fertility problems, many of whose treatment has been unsuccessful elsewhere.
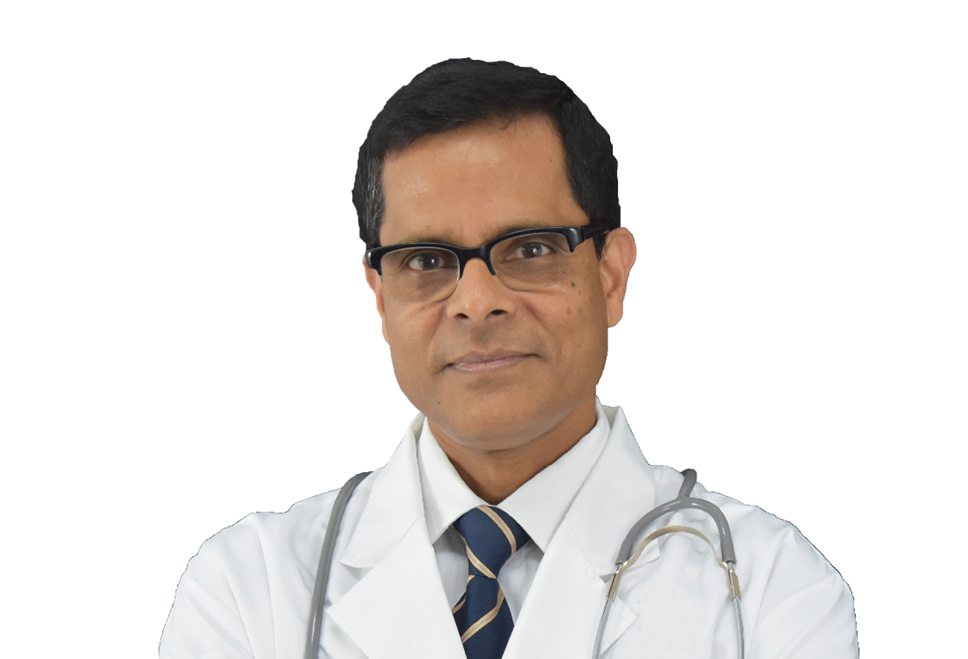
Fertility Centre offers comprehensive range of fertility treatments, and we are committed to providing the best medical and scientific services currently available within this field. The centre coordinator is Dr. Mrinal Kumar Sarker, who is at the forefront of infertility management. Dr. Mrinal and his experienced team of fertility doctors, nurses and embryologists have successfully helped many couples experiencing infertility troubles in fulfilling their dreams of a child.
The first test tube babies (twins) were born at Fertility Centre on 20th April 2009. Since then, more than 300 babies have been born through IVF and many more mothers are expecting. On 17th November 2010, the first birth (twins) through embryo freezing has been accomplished by the centre.
CONSULTATION & APPOINTMENTS
Fertility Centre provides consultation services in level-1 through highly qualified and experienced Consultant, who carefully evaluates each patient. After diagnosing the patient’s condition, our consultant discusses available treatment options and recommends the most effective treatment.
CONTACT INFORMATION OF FERTILITY CENTRE
At Fertility Centre, we maintain total patient privacy and confidentiality. For further details and enquiries, please contact Fertility Centre at the following numbers:
Landline:02-8431661, Ext. – 1212 & 1213
Mobile: 01713041283
List of Doctors
We can help you choose top specialists from our pool of expert doctors, physicians and surgeons.
Conditions Treated
Fertility Centre is well equipped to provide a comprehensive range of fertility treatments. The treatment program to be selected will depend upon the needs and preferences of each individual couple and could consist of one or a combination of the following treatment options. Please click on the links below for a detailed description of each of the treatments:
- OVULATION INDUCTION & CYCLE MONITORING
- INTRA-UTERINE INSEMINATION (IUI)
- IN VITRO FERTILIZATION (IVF)
- EMBRYO TRANSFER
- SURGICAL SPERM RETRIEVAL
- INTRA-CYTOPLASMIC SPERM INJECTION (ICSI)
- BLASTOCYST TRANSFER
- EMBRYO FREEZING & REPLACEMENT OF FROZEN EMBRYOS
- EGG FREEZING
- SEMEN FREEZING
- ENDOSCOPIC SURGERY
OVULATION INDUCTION & CYCLE MONITORING
If a woman has an irregular menstrual cycle, monitoring with ultrasound scans and hormone assessments may help to identify the fertile time of the month and so improve the chances of natural conception.
If ovulation is not occurring, then drugs may be administered after the onset of menstruation to stimulate egg production. The simplest treatment is with tablets given within the first few days of the cycle. The response is monitored by ultrasound scans.
These are not always effective and more powerful fertility injections may be necessary to stimulate egg production in the ovaries. With these more potent drugs there is a greater risk of increased egg production and, therefore, the risks of multiple pregnancies are greater. Women receiving fertility injections are monitored by ultrasound scans and hormone assessment.
INTRA-UTERINE INSEMINATION (IUI)
IUI involves the injection of treated sperm from the husband into the woman’s uterine cavity via the cervix. It is generally a painless procedure which takes only a few minutes and is performed on an out-patient basis. The chances of success are increased if the insemination is combined with ovulation induction using small doses of fertility drugs (15-20% per cycle).
The development of the ovarian follicles is monitored with ultrasound and the insemination is timed to take place 36-40 hours after administration of the hormone injection hCG, which triggers ovulation.
When ovulation has occurred, the male partner is asked to produce a semen sample. This sample is prepared in the laboratory and is then placed in the uterine cavity by means of a soft catheter.
IUI should be performed in cases where the woman has healthy fallopian tubes, and the sperm preparation is satisfactory.
IN VITRO FERTILIZATION (IVF)
IVF is the most effective treatment for women with absent, blocked, or damaged fallopian tubes, for whom it was first developed. It is now used to treat a wide range of fertility problems.
Fertility drugs are used to stimulate the ovaries to produce multiple follicles. Each follicle should contain one egg. The chances of pregnancy are increased if more than one egg can be obtained and fertilized.
The response to stimulation is monitored by ultrasound scan measuring the number and size of the developing follicles in the ovaries and by measuring the blood oestrogen level.
The ultrasound does not show the eggs themselves, but the fluid-filled sacs (follicles) containing the eggs. The ultrasound scans are performed at intervals during the treatment cycle. A typical cycle would require 4 ultrasound scans.
When the leading follicle reaches the optimum size of (17-22mm), preparations will be made for egg collection. An oestradiol assay will also be carried out prior to administering hCG, to help determine the timing of egg collection.
The final preparation for egg collection involves a hormonal injection given to the woman 36-40 hours pre-operatively. This mimics the natural process which triggers the eggs to complete their maturation making them ready for fertilization.
The eggs are collected vaginally using ultrasound guidance, under general or local anaesthesia. The ultrasound probe is introduced into the vagina, the ovaries are visualized and then an aspiration needle (attached to the probe) is passed through the top of the vagina into the follicles.
The fluid in each follicle is aspirated and then examined under a microscope for the eggs to be identified. It is difficult to predict the number of eggs available from the ultrasound scan picture. We therefore frequently collect either more or fewer eggs than we had anticipated pre-operatively.
In rare circumstances we fail to collect any eggs despite the appearance of follicles on the scan picture. If this occurs, the treatment cycle cannot proceed to embryo transfer and you will be given an appointment to see the doctor to discuss your future treatment options.
EMBRYO TRANSFER
After egg collection, the eggs are incubated for a short time and the sperm is then added to the eggs and incubated in the laboratory for a further 18-24 hours. Providing that the semen is normal, approximately 65–75% of the eggs will fertilize on average although it can be highly variable from one cycle to another. The first signs of fertilization are shown by the presence of two pronuclei within the egg.
If this has occurred, the fertilized egg should then divide into two, and subsequently three, four or more cell embryos. The fertilized eggs (now called embryos) are transferred to the uterus 2-5 days after egg collection. A maximum number of two embryos are transferred in women under 40. It is becoming more common for us to transfer embryos at the blastocyst stage (5-6 days after egg collection). In this situation it is recommended that one embryo is transferred due to the increased chance of multiple pregnancy.
It is important that you are aware that there is always a possibility that a low proportion or even none of the eggs fertilize. If this occurs, you will be seen by the clinician to discuss your future treatment options.
The embryo transfer procedure is one of the most important events in IVF. It is generally a painless procedure, similar to a cervical smear and on average takes up to 15 minutes. On rare occasions this procedure may take longer. An abdominal scan is generally performed to confirm the correct position of the transfer catheter within the uterine cavity prior to replacement.
We encourage the male partners to be present during this special time, if they wish to do so. After the procedure, women are encouraged to carry on with their normal routine as there is no evidence to suggest that bed rest has a positive effect. Additional progesterone in the form of vaginal pessaries or injections are given following egg collection until the pregnancy test is done 2 weeks later. If the pregnancy test is positive the progesterone is continued until the second pregnancy scan at 8-9 weeks.
Cancelled treatment cycles
Unfortunately, not all patients respond to the medication and sometimes it may be necessary to abandon the treatment cycle before egg collection. Future management will be discussed, and another treatment cycle may be arranged for a later date, perhaps with a different combination of fertility drugs.
Drugs used in infertility treatment
A variety of drug regimens are used in the treatment cycles and different combinations of drugs may be given to different patients. These combinations may also differ from cycle to cycle. Your doctor will decide which is the most suitable for you.
The basic approach in using these drugs is to suppress the hormones produced by the pituitary gland using a Gn-RH agonist or antagonist, and to stimulate egg production using fertility injections of follicle-stimulating hormone (FSH).
The drugs most commonly used are administered subcutaneously (under the skin) and most women find it easy to inject themselves once they have been taught by our nurses. The Gn RH agonist or antagonist is administered either as a subcutaneous injection or as a nasal spray. All of the drugs used during your treatment are available from our on-site pharmacy. The pharmacy is open 7 days a week and offers competitive prices.
SURGICAL SPERM RETRIEVAL
Surgical sperm retrieval is a treatment option for men with an absence or blockage of the tube (vas deferens) or non-obstructive azoospermia. This is a minor procedure, usually carried as a day case surgery under a local general anesthetic. Surgical sperm retrieval is carried out by a Uroandrologist who works in close association with the Fertility Centre and the procedure is timed to coincide with the female partner’s egg collection.
If enough sperm is retrieved it may be possible to freeze small amounts for use at a later stage. The sperm collected is then used to inject the eggs using ICSI.
There are three methods of surgically retrieving sperm from the testis:
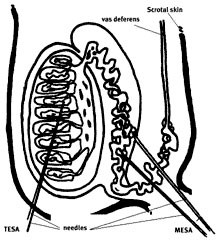
Micro Epididymal Sperm Aspiration (MESA)
MESA involves aspiration of sperm from the epididymis with a fine needle. Sperm collected using this procedure are often of poor quality but are usually suitable for cryostorage. One aspiration may provide enough sperm for several attempts at IVF using ICSI. MESA can be performed well in advance of any proposed IVF procedure.
Testicular Sperm Extraction (TESA)
TESA involves taking a small piece of tissue from the testis and isolating the sperm from the seminiferous tubule. The number of sperm isolated is often very small (usually less than with MESA) and as a general rule these sperm cannot be cryostored. The procedure is thus performed typically twenty-four hours prior to the oocyte collection procedure.
Originally TESE was only performed in cases of non-obstructive azoospermia, however because the procedure can be performed under local anesthetic using a biopsy needle it has become the method of choice for all types of azoospermia. A surgical biopsy may be less damaging to the testis than a needle biopsy and is probably less painful.
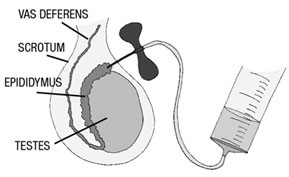
Percutaneous Epididymal Sperm Aspiration (PESA)
PESA is a simple technique to obtain sperm for Intra Cytoplasmic Sperm Injection (ICSI) in men who have an obstruction of the vas deferens, either due to vasectomy or other obstruction. To minimize scarring and damage, PESA usually is attempted on one side only. It is sometimes necessary to aspirate from both sides. Sufficient sperm for ICSI is obtained in 80% of attempts. In 10% of cases enough suitable sperm is found for cryopreservation.
After injection of anaesthetic in the scortum, the doctor will swab the scrotum with a warm antiseptic. The doctor will examine the testes to locate the vas deferens by gently feeling the scrotum. A small needle will be inserted into the vas deferens, and the doctor will instruct the nurse assisting to draw back on the plunger in order to aspirate seminal fluid.
When fluid is obtained, it is passed to the andrologist to be examined for motile (moving) sperm. The procedure may need to be attempted again until motile sperm have been found.
The procedure is usually performed just prior to the woman’s oocyte collection (on the same day). If no sperm is retrieved the oocyte collection may be cancelled.
INTRA-CYTOPLASMIC SPERM INJECTION (ICSI)
ICSI is the injection of a single sperm directly into the egg using a specially prepared needle. It is recommended for severe cases of male infertility and where there has been no fertilization following IVF previously.
With ICSI, very few sperm are required and the ability of the sperm to penetrate the egg is no longer important as this penetration is bypassed by the ICSI technique. It is important to remember that whilst ICSI is a technique used in the laboratory to help fertilization occur, it does not guarantee it. Couples go through the same preparatory processes as with IVF, namely ovulation induction and egg collection.
ICSI can only be carried out on a mature egg. Unfortunately, egg maturity can only be truly identified under the microscope, and it is, therefore, possible that following egg collection, none of the eggs are suitable for ICSI. This situation is fortunately rare.
A small percentage of eggs (fewer than 1 in 10) will be damaged by the injection process and the damage is evident at the time of the injection procedure. These eggs can no longer be used. Of the remaining eggs, however, on average 6 out of 10 are fertilized following the ICSI procedure. The fertilized embryos are allowed to develop as for standard IVF treatment prior to embryo transfer.
Does ICSI carry any risks to our baby?
ICSI, like IVF, is an invasive procedure. However, unlike IVF, ICSI involves injecting a sperm directly into an egg, therefore allowing the use of sperm that may otherwise not be able to fertilize an egg. For these reasons, concerns about the potential risks to children born as a result of ICSI have been raised and there have been a number of follow-up studies carried out.
ICSI is still a relatively new technique and children born as a result of ICSI are still very young. Consequently, these follow-up studies involve relatively small numbers of children and, therefore, the results to date are not conclusive. It has been suggested that ICSI is associated with certain genetic and developmental defects in a small number of children born using this treatment.
We advise that all children conceived as a result of ICSI have regular developmental assessments.
BLASTOCYST TRANSFER
In our centre embryos are usually transferred back into the womb two or three days after eggs have been collected. With the development of new embryo culture media, we have demonstrated that it may be possible to improve the success of IVF and ICSI treatment by delaying the embryo transfer to five or six days after egg collection. These late stage, pre-implantation embryos are called blastocysts.
Which patients will benefit from a blastocyst transfer?
In our centre we will often make the decision to transfer blastocysts depending on the number and quality of embryos available three days after egg collection. For example, if the laboratory team are unable to select the best two embryos for embryo transfer because there are a large number of rapidly developing, good quality embryos on day 3 they may suggest delaying the embryo transfer to day 5 or day 6.
How will it alter my treatment?
Treatment cycles in which blastocysts are transferred are very similar to routine IVF and ICSI cycles. The only difference is that instead of undergoing an embryo transfer on day 2 or day 3 post egg collection it will occur on day five or day six. The embryo transfer procedure itself is the same.
Some patients may not have an embryo transfer because no blastocysts have been formed in the group of embryos that underwent prolonged culture.
Patients having blastocyst transfers in our centre will only be able to have a maximum of two blastocysts transferred. This is because published data indicates that the chances of pregnancy following the transfer of blastocysts are high and therefore there is an increased risk of a multiple pregnancy.
Can I freeze excess embryos?
Yes. As the implantation potential of blastocysts is quite high, we recommend freezing any good quality blastocysts that are not used for the fresh embryo transfer. This means that we will recommend the freezing of single blastocysts.
Are there any risks associated with blastocyst transfers?
The number of blastocyst transfers that have been carried out clinically is still small compared to routine day 2/3 transfers. This means that the risks if any, associated with this technique are unknown. Blastocyst transfers have been carried out for some time in other species.
There is an increase in the incidence of monozygotic (identical) twins. In very few cases there may be some risks associated with these pregnancies. Please speak to one of our doctors or Embryologists should you require further information.
EMBRYO FREEZING & REPLACEMENT OF FROZEN EMBRYOS
Embryos not transferred to the uterus may be suitable for freezing according to the wishes of the couple. We recommend freezing when there are good quality embryos left after the embryo transfer is completed. Poor quality embryos, or embryos which are slow to develop, are unlikely to survive freezing and thawing to give a reasonable chance of pregnancy.
These embryos can be replaced in a future cycle without the woman having to undergo the same drug treatment and surgery. Embryos can be frozen for up to five years, although this can be extended to ten years in exceptional circumstances.
The results following the transfer of frozen-thawed embryos depend on the number and quality of embryos available as well as the age of the woman. Pregnancy rates following frozen embryo transfer are generally lower than after transfer of fresh embryos, but it is much simpler to undertake a frozen embryo cycle. Frozen embryo transfer has been practiced since 1983 and there appears to be no increased incidence of fetal abnormality in babies born following this procedure.
Whether to freeze embryos or not is an important decision for a couple. The couple must give written consent to storage and their future use. It is very important that these are completed accurately as any inconsistencies in the couples’ consent forms may make the storage of the embryos invalid. Patients are also responsible for keeping in touch with the unit and notifying us of any change of address. The storage period is governed by law and we do not need your consent to remove these embryos from storage at the completion of the statutory period.
About 90% of all frozen embryos survive the thawing process. Although some couples may have all of their embryos survive in good condition, others may not have any that survive.
Replacement of frozen embryos is relatively simple. The woman’s natural cycle is monitored to time ovulation using an ultrasound scan and ovulation predictor kits. Following ovulation, the embryos are thawed and transferred back to the uterus. If the woman’s cycle is irregular, we may recommend hormone replacement therapy (HRT), which will allow us to prepare the lining of the uterus for embryo transfer.
EGG FREEZING
Fertility Centre offers egg freezing to women who are facing a total loss of, or a significant decline in, ovarian function, which may have an impact on their future fertility. The work up for egg freezing is similar to that covered in IVF. The difference is that the eggs are frozen and not fertilized. It is usual to perform ICSI on these eggs when they are eventually thawed and used for transfer.
SEMEN FREEZING
Semen freezing is useful for men who find it difficult to ejaculate on demand which may result in their inability to produce a sample on the day of egg collection. By freezing semen prior to treatment, we hope to alleviate some of the stress associated with producing a sample. However, the quality of the semen is reduced after freezing and therefore, if possible, fresh samples are obtained on the day required
ENDOSCOPIC SURGERY
Endoscopic surgery is performed under general anesthetic and includes hysteroscopy and laparoscopy.
Hysteroscopy involves passing a telescope into the uterine cavity through the vagina and the cervix. It is used to inspect the condition of the uterus from within. It can also be used to perform surgical procedures such as the removal of fibroids, polyps or adhesions or to correct congenital abnormalities in the uterus.
Laparoscopy involves an inspection of the pelvic organs by a telescope passed through a tiny incision at the navel. A separate small incision at the level of the pubic hair is used to introduce a probe to manipulate the pelvic organs. It is used to assess the condition of the female pelvis, check whether the fallopian tubes are open and to diagnose the presence or absence of adhesions, endometriosis or other pelvic abnormalities. Surgery can be performed through the laparoscope to treat any of these conditions.
We also perform:
Laparoscopic surgery for tubal infertility
Laparoscopic removal of fibroids
Laparoscopic ovarian diathermy for the treatment of PCOD
Laparoscopic treatment of endometriosis
Hysteroscopic removal of uterine fibroids and adhesions
Laparoscopic removal of ovarian cysts
Open surgery for removal of large fibroids (myomectomy).
IMPORTANT POINTS ABOUT TESTS/PROCEDURES/SURGERIES, YOUR REPORTS & BILLING ENQUIRIES
- Tests/Investigations:
- To schedule a test/investigation, please call the relevant OPD front desks.
- Your lab investigation samples are to be deposited in the Sample Collection Room located in the hospital’s atrium, which is open on working days (Saturday-Thursday) from 7.00 am to 10:00 pm, and on Fridays and holidays from 7.00 am to 6.00 pm.
- Your investigation reports can be collected from Report Delivery Room by showing the receipt of payment. The hospital shall not be responsible for reports not collected within 30 days after the tests were done. Report Delivery Room is also located in the hospital’s atrium, and is open on working days (Saturday-Thursday) from 8.00 am to 8.30 pm, and on Fridays and holidays from 9.00 am to 5.00 pm.
- You will not be able to collect your investigation reports without your receipt of payment. If you have lost your receipt, you may collect a duplicate copy from our Billing Executives (Corporate Desk, Atrium – level 1).
- You can request duplicate copy of your investigation reports from the Report Delivery Room, inclusive of BDT 100 additional charge.
- Procedures & Surgeries:
- If you are interested in undergoing a procedure or surgery, please see our relevant Consultant first.
- To search for a Consultant, go to Find a Consultant page and for appointments, go to Make an Appointment
- In-patient Reports
- A Discharge Summary is provided to a patient upon his/her discharge from the hospital. A discharge summary is a summary of the events during hospitalization of the patient. It outlines the patient’s chief complaint, the diagnostic findings, the therapy administered and the patient’s response to it, and recommendations on discharge.
- To request for detailed in-patient medical reports or to make an insurance claim, refer to our Medical Report
- For queries on charges, contact our Billing Department (Corporate Desk, Atrium – level 1) or call/e-mail our Billing Executives:
| Mr. Taslimur Rahman: AGM – Financial Operation Phone : +88-02-8431661-5; Ext-1353 (From 9 am to 5 pm –Except Holidays) E-mail: taslimur.rahman@evercarebd.com |